07/08/2024
07/08/2024
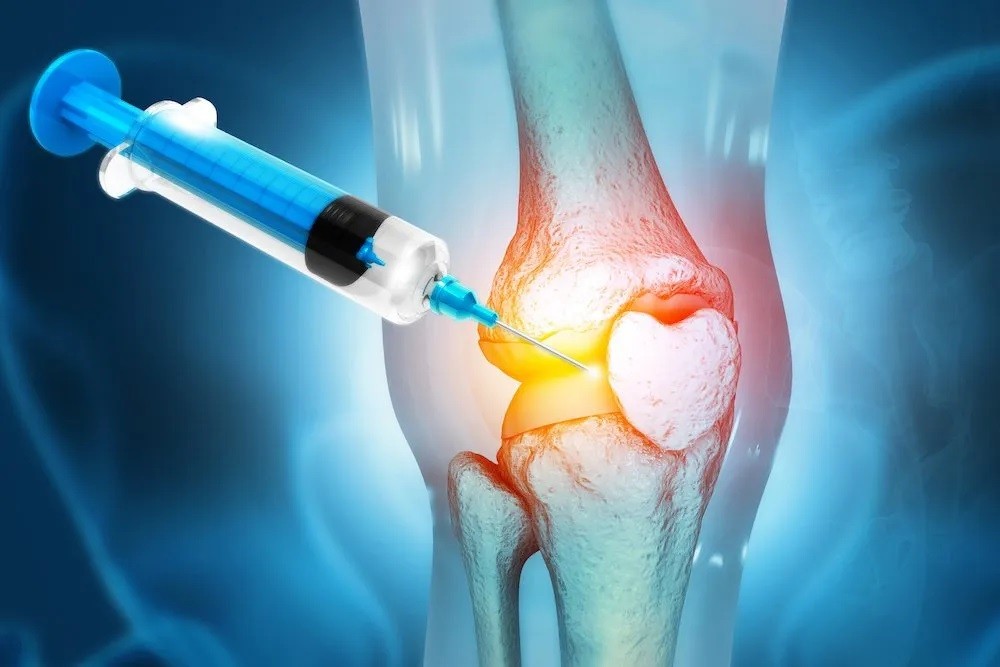
NEW YORK, Aug 7: Scientists have developed an innovative injectable "goo" (biomaterial) capable of regenerating cartilage, offering potential future treatments for joint damage. Although currently tested only in sheep, the research promises significant advancements in treating degenerative diseases like osteoarthritis and sports-related injuries such as anterior cruciate ligament (ACL) tears.
Cartilage, a vital tissue that cushions joints and prevents bone friction, deteriorates with age or injury, often leading to joint pain and mobility issues. Unlike other tissues, cartilage lacks an active blood supply, making natural healing difficult and often necessitating surgical intervention.
Microfracture surgery is a common treatment for damaged cartilage, involving the removal of damaged tissue and drilling holes in the underlying bone to stimulate cartilage growth. However, the new cartilage, fibrocartilage, is generally weaker and less durable than the original hyaline cartilage.
In a study published on August 5 in the journal PNAS, researchers from Northwestern University's Simpson Querrey Institute for BioNanotechnology, led by Samuel Stupp, introduced a groundbreaking injectable biomaterial designed to regenerate hyaline cartilage. This biomaterial incorporates a protein that attracts transforming growth factor-beta1 (TGF-b1), a chemical that promotes cartilage repair, and hyaluronic acid, which encourages stem cell differentiation into cartilage.
The team tested the biomaterial on sheep with stifle joint defects—a joint similar to the human knee. Within six months of a single injection, significant cartilage growth and repair were observed, outperforming injections of TGF-b1 alone. The newly formed cartilage in the treated sheep closely resembled natural hyaline cartilage.
Looking ahead, researchers aim to further develop the biomaterial for human applications, with hopes of providing a durable solution to joint pain and poor mobility. “Our approach should be more resistant to wear and tear compared to microfracture surgery,” said Stupp. The ultimate goal is to reduce the need for extensive joint reconstruction and potentially avoid full knee-replacement surgeries.
The progress in this research marks a promising step towards improving joint health and mobility in the long term.


