22/01/2024
22/01/2024
NEW YORK, Jan 22: Cynthia Horton, 61, battles excruciating ear infections, a consequence of antibiotic-resistant bacteria. The global rise of drug-resistant superbugs has led researchers to explore innovative solutions. Phage therapy, employing microscopic viruses called bacteriophages, is emerging as a potential game-changer.
Horton's struggle intensified after a 2003 cancer surgery, leaving her immune system weakened by radiation and chemotherapy. Over the years, her ear infections became resistant to antibiotics, prompting doctors to consider phage therapy—a treatment that deploys viruses to target and eliminate bacteria.
Superbugs, responsible for over 2.8 million antimicrobial-resistant infections annually in the United States, pose an urgent global public health threat. By 2050, an estimated 10 million people per year could succumb to superbug infections, highlighting the critical need for alternative therapies.
In a surprising turn, samples from Horton's ear revealed a rare superbug strain linked to contaminated over-the-counter eye drops causing severe infections. This discovery prompted scientists to investigate if phages, cultivated from Horton's ear bacteria, could combat these eye infections.
An outbreak of antibiotic-resistant eye infections emerged in May 2022, affecting at least 50 patients across 11 states. By January the following year, the CDC reported the outbreak's escalation, with 18 states affected, resulting in deaths, vision loss, and infections in various body parts.
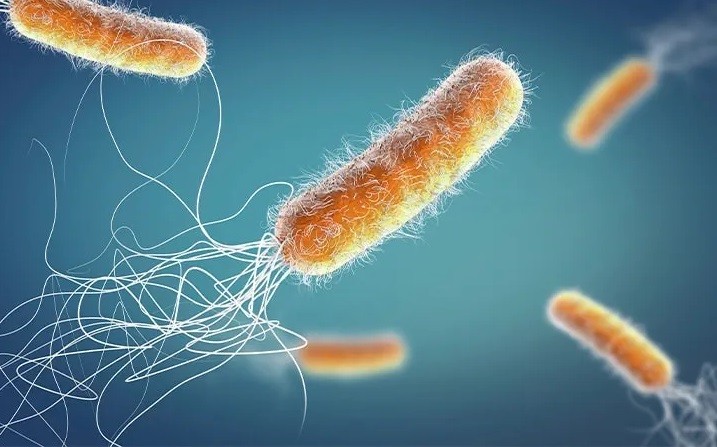
The superbug strain, a rare drug-resistant Pseudomonas aeruginosa, had not been previously identified in the US. The bacteria cultured from Horton's ear matched the strain, leading to the swift identification of phages capable of attacking the deadly pathogen.
The CDC acknowledged the significance of phage therapy, highlighting its potential during outbreaks with limited treatment options. As research advances, phage therapy may become vital in the fight against superbugs, revolutionizing infectious disease treatment.
Scientists nationwide are entering the era of "phage 3.0," exploring advanced applications. Research includes mapping phage-antibiotic symbiosis, investigating immune responses, and developing phage libraries for various infections. Clinical trials are underway for conditions like urinary tract infections, cystic fibrosis-related infections, and chronic diseases.
Genetic engineering of phages allows customization for individual patients, offering a targeted approach against antibiotic-resistant pathogens. This advancement could reshape treatment strategies, moving away from traditional sources like sewage and ponds.
The potential of phage therapy has captured the attention of the CDC, suggesting its use not only in outbreak response but also in preventing reinfection. By "decolonizing" bacterial populations in high-risk individuals, phages could reduce infection likelihood and transmission.
Phage therapy represents a beacon of hope in the ongoing battle against antibiotic resistance, showcasing the promise of these microscopic warriors in reshaping the future of infectious disease treatment.


